Abstract
Background:
IgD multiple myeloma (MM) is a rare subtype contributing 2% of all multiple myeloma cases. Despite difficulty and delay in diagnosis, recent advances in the treatment of multiple myeloma in general also improved the outcomes for IgD myeloma subtype. The aim of this study is to summarize the data on presentation patterns, diagnosis, management approaches and outcomes for patients (pts) with IgD myeloma.
Methods:
A comprehensive literature search for articles published after December 2013 was performed using four databases: PubMed, Embase, Cochrane, and Clinicaltrials.gov. With initial search we identified 209 articles and after screening by two independent reviewers we included only 8 studies in the final analysis.
Results:
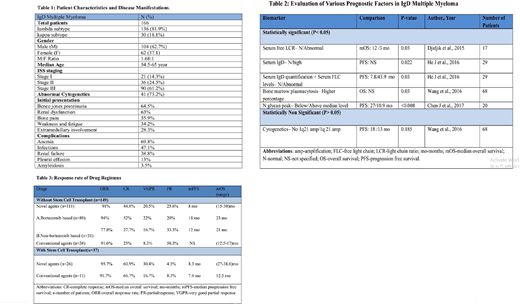
A total of 166 pts with IgD MM were included from 8 selected retrospective case series. Lambda (λ) was the predominant light chain sub-type in 136 patients (81.9%). Initial manifestations of IgD MM were Bence jones proteinuria (BJP>2 g/day-64.5%), renal dysfunction (63%), bone pain (55.9%), weakness, fatigue (34.2%) and extra medullary involvement (28.3%). Renal function was assessed by estimated glomerular filtration rate (eGFR<60 ml/min/1.73m2) in 54.3 % of patients and by serum creatinine level (Cr >2mg/dl) in 46.1% patients. Cytogenetic karyotype analysis in 56 pts using fluorescence in-situ hybridization (FISH) identified abnormal cytogenetics in 41 (73.2%) patients, cases were further classified as high risk (85.7%) and standard risk (14.3%). The patient characteristics and disease manifestations are mentioned in Table 1.
Serum protein electrophoresis (SPEP) showed positive monoclonal spike (M) spike in 84% of the patients. The median M spike value for IgD MM was 9.42 g/l in a cohort of 17pts, (Djidjik et al.) which was lower as compared to IgG (median: 35 g/L) and IgA (median: 32 g/L) in this study. Abnormal serum free light chain ratio (sFLCR) was observed in 83% pts. Quantitative serum IgD levels were elevated only in 28% of the cases. Bone marrow (BM) plasmacytosis showing > 40% abnormal plasma cells was detected in 95.6% of the patients. N glycans are newly discovered biomarkers used for detecting abnormal protein glycosylation in MM patients. NG1(6)A2F and NG1(3)A2F were the two most significant N glycan markers for IgD MM patients with sensitivity of 95% & 95.2%, respectively and specificity of 95% & 78.6%, respectively. The prognostic significance of several other biomarkers studied in IgD MM is mentioned in Table 2.
Treatment details were available for 149 patients and overall response rate (ORR) was seen in 125 (83.9%) patients while 24 (15.4%) patients had progressive or stable disease. The median overall survival (mOS) was between 9 - 62 months. Novel agents (NA) such as bortezomib, thalidomide and lenalidomide were given to 111 (74.4%) pts with the mOS between 15 - 38.6 months. Conventional agents (CA) such as melphalan, vinblastine, vincristine, epirubicin, and ifosfamide were given to 38 (25.5%) patients with mOS between 12.5 - 17 months. Data showed bortezomib based regimens resulted in a higher ORR (ORR=94%, CR=52%) compared to non bortezomib based regimens (ORR=77.8%, CR=27.7%) respectively. Stem cell transplant (SCT) was used in 37 (24.8%) patients with chemotherapy (NA=26, CA=11) which showed good response rate (ORR>90%,CR >60%). The comparison of response rate with different drugs is mentioned in the Table 3.
Conclusion:
N-glycan assay can overcome the limitations of SPEP and quantitative serum IgD assay in the diagnosis of IgD MM. This difficulty is posed by the lower concentrations of M spike ( SPEP) or lower-normal serum IgD value on quantitative serum assays, which can delay its diagnosis. Novel and conventional agents have good responses with ORR>90%, but mOS of conventional agents was lower when compared to novel agents. Bortezomib based regimens showed better responses when compared to non-bortezomib regimens. The best response (ORR=95%) was obtained with use of SCT in combination with novel agents. Serum free light chain levels, N glycan assay and serum IgD quantification were found to be the best prognostic markers for IgD MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal